Migraines are far more than mere headaches. For many, they arrive like an uninvited storm, pounding temples, vision disturbances, nausea, and days lost to darkened rooms and silence. Understanding what causes migraines in females is a step towards reclaiming those lost hours and reshaping daily life.
In cities like Chennai, where modern medicine meets tailored therapies, solutions have become more holistic. The approach is no longer restricted to quick relief; it’s about understanding why migraines occur and what can be done to stop them before they start.
What Causes Migraines in Females?
Women are statistically three times more likely to experience migraines compared to men. This isn’t a coincidence; it’s chemistry, biology, and environment converging. Hormones play a leading role, but so do emotional health, sleep quality, and reproductive milestones. No two stories are the same, which is why recognising one’s triggers can be empowering.
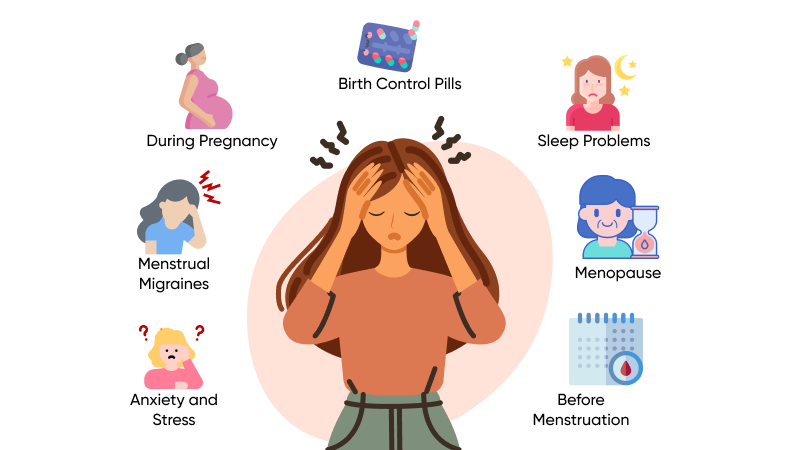
Anxiety and Stress
Life’s constant tug-of-war often leaves women carrying invisible loads. When cortisol levels rise and remain elevated, they affect blood flow and neurological patterns, both of which contribute to migraine development.
Stress isn’t always loud. It can be subtle—sleepless nights, decision fatigue, feeling rushed without pause. Over time, this builds into a fertile ground for recurring headaches. Breath work, reflective journaling, and mindfulness exercises offer quiet but powerful buffers.
Menstrual Migraines
Hormonal fluctuation is one of the most cited reasons behind migraines in women. For some, the onset of menstruation acts as a biological switch, triggering episodes that arrive with precision. The sudden drop in oestrogen levels just before a period is believed to lower the threshold for pain signals, making the nervous system more reactive.
The pain linked to this shift often settles on one side of the head, accompanied by sensitivity to light, fatigue, or mood changes. Keeping a menstrual and migraine journal often reveals patterns that are otherwise easy to overlook. Tailored treatment, when designed in sync with the menstrual cycle, can significantly reduce frequency and severity.
During Pregnancy
Pregnancy introduces dramatic hormonal changes, and the effects vary widely among individuals. Some women experience fewer migraines during this phase, especially during the second and third trimesters. For others, particularly in the early months, migraines may increase due to rising oestrogen levels, disrupted sleep, or changes in blood sugar levels.
Managing these episodes without medication can be challenging. This is where the expertise of pain management doctors in Chennai becomes invaluable. Safe techniques such as nerve stimulation therapy, hydration therapy, and postural guidance can offer relief without compromising maternal or foetal health.
Birth Control Pills
Synthetic hormones, especially those in oral contraceptives, can trigger headaches in women sensitive to hormonal shifts. Migraine episodes often begin or worsen in those who start or change hormonal birth control methods. The timing of migraines, especially during the pill-free interval, can point directly to the oestrogen withdrawal effect.
Collaborating with medical professionals familiar with women’s health and neurology helps identify options that support balance.
Sleep Problems
Good sleep is restorative; poor sleep is disruptive. This is especially true for women managing migraines. Irregular sleep schedules, insomnia, or even oversleeping can alter the brain’s pain-regulating chemicals. When deep sleep is disturbed repeatedly, the brain struggles to manage stimuli, increasing susceptibility to migraine attacks.
At Epione, a pain management clinic in Chennai, strategies include circadian rhythm retraining, posture adjustment for sleep, and ambient therapy. These techniques create the conditions for quality rest without dependence on pills.
Menopause
The approach to menopause is marked by hormone instability, with oestrogen levels swinging unpredictably. This transition can worsen migraines in some women, especially during the perimenopausal years.
Once full menopause sets in and hormone levels stabilise, some women report fewer attacks. Until then, gentle interventions such as dietary shifts, acupuncture, and regular physical movement—rather than intense workouts—can help the body cope better.
Before Menstruation
The days leading up to menstruation are when many women experience what’s often called a “silent build-up.” Headaches may seem to come out of nowhere, but in truth, they’ve been set in motion days prior. Triggers such as fluid retention, increased sensitivity to noise or light, and changes in serotonin levels all play a role.
Tracking these symptoms helps anticipate and reduce the impact. Preventive care, hydration, magnesium-rich meals, and daily breathing rituals can soften the body’s reaction to these internal changes.
Conclusion
Migraines aren’t a minor inconvenience. They are complex, often invisible, and deeply influenced by life stages and hormonal realities. Knowing what causes migraines creates space for personalised care, not generic fixes.
By working with the best doctor for migraine in Chennai, patients gain access to diagnostic insight, lifestyle adjustments, and innovative, non-invasive support options.
With focused care and the support of a dependable migraine headache treatment in Chennai, women no longer have to live under the shadow of uncertainty.